Mastering Tracheostomy: A Comprehensive Guide for Healthcare Professionals
- Jadumani Singh

- Dec 10, 2025
- 2 min read
Updated: Jan 5
The Importance of Tracheostomy in Critical Care
Performing a tracheostomy is one of the most critical skills in acute and critical care medicine. It provides an alternative airway for patients who require prolonged ventilation or have upper airway obstruction. Over the years, the percutaneous tracheostomy has become the preferred method in many intensive care units, valued for its minimally invasive technique and bedside feasibility.
Understanding the Tracheostomy Procedure
A tracheostomy involves creating an opening in the neck to insert a tube directly into the trachea. This allows air to bypass obstructions or facilitate long-term ventilation. The percutaneous technique is commonly performed under local anaesthesia with sedation, making it suitable for ICU settings.
Key Steps in the Procedure
Patient Preparation: Confirm the indication, obtain informed consent, and position the patient in a supine position with the neck extended.
Instrument Preparation: Gather a portable disposable bronchoscope and a difficult airway trolley.
Anatomical Identification: Palpate the cricoid cartilage and identify the tracheal rings, marking the site between the second and third rings.
Local Anaesthesia & Incision: Administer local anaesthetic and make a small horizontal incision.
Needle Insertion & Guidewire Placement: Insert a needle into the trachea under aspiration, then advance a guidewire.
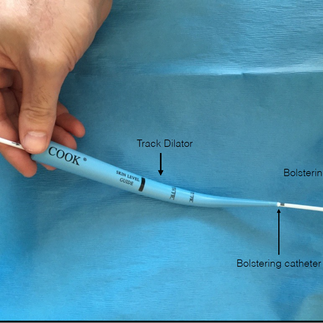
Dilation & Tube Insertion: Use serial dilators or a single tapered dilator over the guidewire before inserting the tracheostomy tube.
Confirmation & Securing the Tube: Confirm placement using auscultation and capnography, then secure and dress the site.
Each step requires precision, effective team coordination, and a thorough understanding of airway anatomy.
⚠️ Safety Considerations
Performing a tracheostomy safely requires more than just technical skill; it demands preparation and situational awareness.
Patient Selection: Avoid performing the procedure on patients with distorted anatomy, infection at the site, or coagulopathy.
Ultrasound Guidance: This enhances accuracy and reduces complications.
Team Dynamics: A skilled operator, assistant, and monitoring personnel are essential.
Sterile Technique: Maintaining a sterile environment is crucial to minimise infection risk.
Emergency Preparedness: Always have rescue airway equipment on hand.
Maintaining these standards ensures safety and procedural success.
🏥 Post-Procedure Care
Ongoing tracheostomy care is crucial to prevent complications and promote healing.
Daily Stoma Care: Regular dressing changes are essential.
Humidified Oxygen: This protects the mucosa and maintains comfort.
Careful Suctioning: Clear secretions to prevent blockage.
Monitoring: Watch for bleeding, infection, or displacement.
Patient and Caregiver Education: Provide guidance for long-term management.
These practices shorten hospital stays, reduce infection risk, and improve patient comfort.
💻 The Role of Technology and Digital Training
Technology continues to transform procedural medicine, and tracheostomy is no exception. Ultrasound imaging, digital documentation, and simulation-based e-learning have made training safer and more accessible.
I encourage you to watch the recorded webinar on percutaneous tracheostomy for further insights. You can find it here.
Conclusion
In conclusion, mastering the tracheostomy procedure is essential for healthcare professionals in critical care settings. By understanding the steps involved, prioritising safety, and embracing technology, we can enhance patient outcomes and ensure effective airway management. The integration of digital health solutions is vital for improving patient care and operational efficiency.







Comments